Can you get social security disability for sleep apnea?
Sleep apnea is a common yet often misunderstood condition. It affects millions worldwide, disrupting sleep and impacting daily life.
But is sleep apnea a disability? This question is more complex than it seems. It requires a deep understanding of both medical and legal perspectives.
In this article, we explore the intricacies of sleep apnea, including its symptoms, health consequences, and diagnostic criteria.
We also examine the legal definitions of disability. We discuss how sleep apnea fits within these frameworks, including the Americans with Disabilities Act and Social Security disability benefits.
We aim to understand sleep apnea as a potential disability comprehensively. We hope this information will be valuable to those affected by sleep apnea, their families, healthcare professionals, and disability advocates.
What is Sleep Apnea?
Sleep apnea is a sleep disorder. It is characterized by repeated interruptions in breathing during sleep. These interruptions, known as apneas, can occur hundreds of times in a single night.
Each apnea event can last from a few seconds to over a minute. During this time, the brain and the rest of the body may not get enough oxygen. This can lead to a range of health problems.
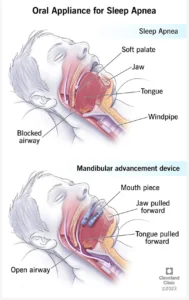
The primary cause of these interruptions is a blockage in the airway, which can be partial or complete. Relaxing the muscles in the back of the throat often causes this blockage.
The key symptoms of sleep apnea include:
- Excessive daytime sleepiness
- Loud snoring
- Observed episodes of stopped breathing during sleep
- Abrupt awakenings accompanied by gasping or choking
- Morning headache
- Difficulty concentrating during the day
- Mood changes, such as depression or irritability
- High blood pressure
- Nighttime sweating
- Decreased libido
Types of Sleep Apnea
There are three main types of sleep apnea: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome.
Obstructive sleep apnea is the most common form. It occurs when the muscles in the back of the throat relax excessively. This causes the airway to narrow or close as you breathe in, leading to apnea events.
Central sleep apnea (CSA) is less common. It occurs when the brain fails to signal to the breathing muscles properly. Unlike OSA, CSA is not caused by a physical airway blockage.
Complex sleep apnea syndrome is a combination of both OSA and CSA. It is also known as treatment-emergent central sleep apnea. It occurs in some people who have OSA and start using a continuous positive airway pressure (CPAP) machine.
Symptoms and Health Consequences
Sleep apnea can have serious health consequences if left untreated. It can lead to several cardiovascular problems, including high blood pressure, heart disease, and stroke.
People with sleep apnea are also at a higher risk of developing insulin resistance and type 2 diabetes. They may experience liver problems, including nonalcoholic fatty liver disease. Sleep apnea can also contribute to metabolic syndrome, a cluster of conditions that increase the risk of heart disease.
The repeated awakenings associated with sleep apnea make normal, restorative sleep impossible. This leads to excessive daytime sleepiness, which can interfere with daily activities and increase the risk of accidents.
Furthermore, untreated sleep apnea can lead to severe complications with medications and surgery. People with sleep apnea may also experience changes in mood, including depression and anxiety. These psychological effects can further impact the quality of life and overall health.
Legal Definitions and Criteria for Disability
In the legal context, a disability is a physical or mental impairment. This impairment must substantially limit one or more major life activities. The definition also includes individuals who have a history of such an impairment or are perceived by others as having such an impairment.
Under this definition, sleep apnea can be considered a disability. It can substantially limit major life activities, such as breathing and sleeping, and can lead to other health problems that may further limit these activities.
However, not all cases of sleep apnea will qualify as a disability. The severity of the condition and its impact on the individual's life are key factors. The individual must be unable to perform substantial gainful activity due to their impairment.
The determination of disability is not based solely on medical evidence. Non-medical evidence, such as the individual's statements and information from family, friends, and others, can also be considered.
The Americans with Disabilities Act (ADA) and Sleep Apnea
The Americans with Disabilities Act (ADA) prohibits discrimination against individuals with disabilities. This includes individuals with sleep apnea if their condition substantially limits a significant life activity.
Under the ADA, employers must provide reasonable accommodations for employees with disabilities. For individuals with sleep apnea, this could include modifications to work schedules or duties or the provision of special equipment.
However, to be protected under the ADA, an individual must be able to perform the essential functions of their job, with or without reasonable accommodation. They must also not directly threaten the health or safety of others in the workplace.
Social Security Disability Benefits for Sleep Apnea
The Social Security Administration (SSA) provides disability benefits for individuals unable to work due to a medical condition. Sleep apnea can qualify for these benefits, but the criteria are strict.
To qualify, an individual must have a severe form of sleep apnea that meets the SSA's listing of impairments. The listing for sleep apnea includes specific criteria related to the frequency of apnea events and other health problems.
The SSA also considers the individual's residual functional capacity (RFC), which assesses their ability to sustainably engage in physical and mental work activities despite their impairment.
The SSA's criteria for disability benefits due to sleep apnea include:
- Evidence of chronic sleep apnea with episodes of apnea or hypopnea documented by sleep testing
- Cor pulmonale (right-sided heart failure) or pulmonary vascular hypertension (high blood pressure in the lungs) resulting from sleep apnea
- Severe daytime sleepiness resulting in an inability to function in a work setting
VA Disability Ratings for Sleep Apnea
The Department of Veterans Affairs (VA) recognizes sleep apnea as a disability for veterans. It assigns a disability rating based on the severity of the condition and its impact on the veteran's life.
The VA uses a rating schedule to determine the percentage of disability, which determines the amount of compensation the veteran will receive.
The VA rating can range from 0% to 100% for sleep apnea. A 0% rating means that the condition is recognized but does not warrant compensation. A 100% rating means the condition is so severe that it impairs the veteran's ability to work.
The VA considers several factors in assigning a disability rating for sleep apnea. These include the frequency and severity of apnea events, related health problems, and the condition's impact on the veteran's daily activities and quality of life.
Diagnosing Sleep Apnea as a Disability: prevents you from working
Diagnosing sleep apnea as a disability involves a comprehensive evaluation. This includes a detailed medical history, physical examination, and specialized tests. The most common test is a sleep study or polysomnography.
Various physiological parameters are monitored during a sleep study. These include brain activity, eye movements, heart rate, and breathing patterns. A key measure is the number of apnea and hypopnea events per hour, known as the Apnea-Hypopnea Index (AHI).
A high AHI indicates severe sleep apnea. However, the AHI alone is not sufficient to determine disability status. The impact of sleep apnea on the individual's daily activities and quality of life is also considered.
Other factors, such as other health problems and the individual's response to treatment, can influence the disability determination and the AHI.
Medical Documentation and Expert Testimony: Meet the Criteria
Medical documentation is crucial in establishing sleep apnea as a disability. This includes medical records, test results, and statements from healthcare providers. These documents provide objective evidence of the condition and its impact.
Expert testimony can also be significant. Sleep specialists and other healthcare providers can provide valuable insights into the severity of the condition and its effects on an individual's life.
These experts can explain the medical complexities of sleep apnea. They can also discuss the individual's symptoms, treatment response, and limitations. Their testimony can help clarify how sleep apnea impairs the individual's ability to perform major life activities.
However, the individual's testimony is also essential. Their account of their symptoms, struggles, and limitations can provide a compelling case for sleep apnea as a disability.
Treatment and Management of Sleep Apnea
Treatment for sleep apnea aims to alleviate symptoms and reduce health risks. The most common treatment is Continuous Positive Airway Pressure (CPAP). This device delivers pressurized air through a mask, keeping the airway open during sleep.
However, only some people tolerate CPAP well. Alternatives include oral appliances, positional therapy, and, in some cases, surgery. Treatment choice depends on the severity of sleep apnea and the individual's health.
Managing sleep apnea also involves addressing associated health conditions, such as obesity, hypertension, and diabetes. Regular follow-up with healthcare providers is crucial to monitor the condition and adjust treatment as needed.
Compliance with treatment is key to managing sleep apnea. It can significantly improve the quality of life and reduce the impact of sleep apnea as a disability.
Lifestyle Changes and Assistive Technologies
Lifestyle changes can also help manage sleep apnea. Weight loss, regular exercise, and avoiding alcohol and sedatives can reduce symptoms. Positional therapy, which involves altering sleeping positions, can also be beneficial.
Assistive technologies can help manage sleep apnea. For example, special pillows or devices can help maintain a side-sleeping position, reducing the frequency of apnea events.
Various apps and devices can monitor sleep and provide feedback, helping individuals understand their sleep patterns and make necessary adjustments.
While lifestyle changes and assistive technologies can help, they are usually part of a comprehensive treatment plan and are not typically sufficient alone to manage severe sleep apnea.
Challenges and Considerations in Disability Claims for Sleep Apnea
Claiming disability for sleep apnea can be challenging. The process often requires extensive medical documentation and expert testimony. It's crucial to demonstrate the impact of sleep apnea on daily activities and overall quality of life.
The Social Security Administration (SSA) evaluates disability claims using a specific set of criteria. For sleep apnea, the SSA considers the severity of the condition, the individual's residual functional capacity, and the impact on their ability to work.
Qualify for disability benefits
The Veterans Affairs (VA) also has a specific rating system for sleep apnea. Veterans must show that their sleep apnea is connected to their military service. This can be a complex process requiring medical and legal expertise.
Despite these challenges, it's important to remember that sleep apnea can be a serious condition. It can significantly impact an individual's health and quality of life, and in some cases, it may qualify as a disability.
Psychological Effects and Quality of Life
Sleep apnea can have significant psychological effects. It's associated with increased rates of depression and anxiety. These mental health conditions can further impact an individual's quality of life and may be considered in disability assessments.
The intermittent sleep disruptions caused by sleep apnea can lead to excessive daytime sleepiness. This can affect concentration, productivity, and the ability to perform daily tasks. It can also increase the risk of accidents, including motor vehicle crashes.
The impact of sleep apnea on quality of life is a key consideration in disability claims. It's essential to document these effects and seek appropriate treatment. Mental health support and counseling may be beneficial for individuals dealing with the psychological effects of sleep apnea.
The Role of Advocacy and Support Networks
Advocacy groups and support networks are crucial in raising awareness about sleep apnea. They provide resources and support for individuals navigating the disability claims process and advocate for policy changes to recognize sleep apnea as a disability.
These groups can provide valuable information and guidance. They can help individuals understand their rights and navigate the complex disability claims process. They can also connect individuals with legal and medical experts specializing in sleep apnea and disability law.
Support networks can also provide emotional support. Living with sleep apnea can be challenging, and connecting with others who understand the experience can be beneficial. Online forums, support groups, and social media platforms can provide a sense of community and shared understanding.
Advocacy and support networks are an essential resource for individuals with sleep apnea. They can provide information, support, and a sense of community. They can also play a key role in shaping the future of sleep apnea as a recognized disability.
Conclusion: The Future of Sleep Apnea as a Recognized Disability
The recognition of sleep apnea as a disability is a complex issue involving medical, legal, and societal considerations. As our understanding of sleep apnea continues to evolve, so will its status as a recognized disability.
Advancements in research and technology are likely to play a significant role. They may lead to improved diagnostic tools, more effective treatments, and a better understanding of sleep apnea's impact on daily life. These developments could influence disability assessments and policy decisions.
In the meantime, advocacy and education remain crucial. They can help ensure that individuals with sleep apnea receive the recognition, support, and treatment they need.
Here at Houston Sleep Associates (HSA) in Houston, TX, we are passionate about quality sleep. Our years of experience ensure that each patient receives the best care customized to their unique needs and desires!
Schedule a consultation in Houston, Texas.
See what we offer if you've ever thought about improving your sleep. Schedule a consultation and experience the warmth, professionalism, and transformative power of sleep at HSA. Your journey to a brighter, more confident day begins with a single step. Let's take it together!
Other Sleep Articles:
Revolutionizing Sleep: CPAP Machines Without Mask (houstonsleepassociates.com)
Exploring the Genetic Link to Sleep Apnea - Houston Sleep Associates
Is Sleep Apnea a Disability? Exploring the Complexity (houstonsleepassociates.com)
What happens if sleep apnea goes untreated? - Houston Sleep Associates
Improving Sleep Quality with Mouth Guards - Houston Sleep Associates
Understanding the Science Behind Sleep Apnea Mouth Guards (houstonsleepassociates.com)
The Link Between Weight Gain and Snoring - Houston Sleep Associates

